Ventral Hernia
Ventral Hernia Repair ( Laparoscopic Ventral Hernia )
 Incisional Hernia, Ventral Hernia, Epigastric Hernia, or Umbilical Hernia are defects of the anterior abdominal wall. They may be congenital (umbilical hernia) or acquired (incisional). Incisional hernias form after surgery through the incision site or previous drain sites, or laparoscopic trocar insertion sites. Incisional hernias are reported to occur in approximately 4-10% of patients after open surgical procedures. Certain risk factors predispose patients to develop incisional hernias, such as obesity, diabetes, respiratory insufficiency ( lung disease), steroids, wound contamination, postoperative wound infection, smoking, inherited disorders.
Incisional Hernia, Ventral Hernia, Epigastric Hernia, or Umbilical Hernia are defects of the anterior abdominal wall. They may be congenital (umbilical hernia) or acquired (incisional). Incisional hernias form after surgery through the incision site or previous drain sites, or laparoscopic trocar insertion sites. Incisional hernias are reported to occur in approximately 4-10% of patients after open surgical procedures. Certain risk factors predispose patients to develop incisional hernias, such as obesity, diabetes, respiratory insufficiency ( lung disease), steroids, wound contamination, postoperative wound infection, smoking, inherited disorders.
These hernias present much the same way inguinal hernias do. That is, they present with a bulge near or at a previous incision. Some patients may experience discomfort, abdominal cramping, complete intestinal obstruction, or incarceration as a result of these hernias.
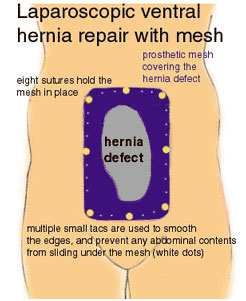
The principle of surgical repair entails the use of prosthetic mesh to repair large defects in order to minimize tension on the repair. A tension free repair has a lesser chance of hernia recurrence. Traditionally, the old scar is incised and removed, and the entire length of the incision inspected.
Generally, there are multiple hernia defects other than the one(s) discovered by physical examination. The area requiring coverage is usually large and requires much surgical dissection. A prosthetic mesh is used to cover the defect(s), and the wound closed. This is a major surgical procedure and often complicated. Infection rates following repair may be as high a 7.0%. Recurrence can be up to 5%, or higher, depending on the patient’s preoperative risk factors.
While the use of prosthetic mesh has decreased the number of recurrences, it has also been implicated in increased infection rates, adhesion or scar formation of the abdominal contents to the anterior abdominal wall leading to intestinal obstruction and fistula formation. However, overall, recovery is usually excellent and patients return to normal activity within a matter of weeks.
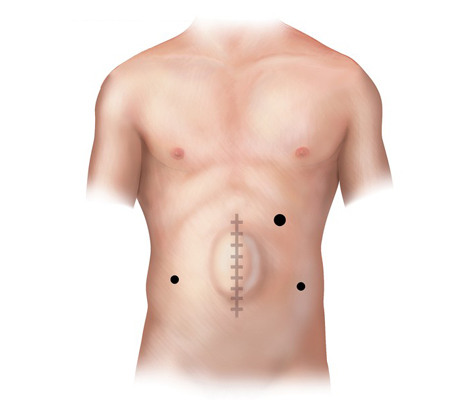
The laparoscopic repair of ventral hernias was designed to minimize operative trauma to the patient. As mentioned, these are often complicated repairs requiring large incisions and extensive tissue dissection.
The principles governing a laparoscopic ventral hernia repair are based on those of open Stoppa ventral hernia repair. A large piece of prosthetic mesh is placed under the hernia defect with a wide margin of mesh beyond the defect. The meshes is anchored in place with full thickness sutures and secured to the anterior abdominal wall with a varying number of tacs, placed laparoscopically.
A patient is a candidate for laparoscopic incisional hernia repair if he/she are medically able to undergo general anesthesia. Also, the defect must “allow” the surgeon to place the laparoscopic trocars in such positions that repair are ergonomically possible. In some very large or giant hernias, the abdominal wall is distorted to such a degree that it is impossible to safely place laparoscopic trocars. Ancillary studies, such as CT scan/MRI of the abdomen and pelvis are helpful in making this decision. Patients are also given a bowel preparation to evacuate the colon and decrease the number of intestinal bacteria prior to surgery.
Patients are admitted the same day of their surgery. Following the procedure and recovery from anesthesia, they are taken to a hospital room where they spend the night. We encourage our patients to move as quickly as possible. It is extremely important to be active early in order to stave off some of the complication seen postoperatively, such as pneumonia, deep venous thrombosis and pulmonary embolism (clots in the legs that break off and go the lungs). Postoperative pain is variable, and can be considerable during the first 24 hours. As such, patients are given I.V. narcotics as needed, and are changed to oral analgesics the next day.
Generally, most patients stay in the hospital 1 or 3 days following surgery. Patients are then seen, by the surgeon, one to two weeks after discharge. There is no dietary restriction. Activity level is restricted by the patient’s comfort level. However, it is generally not advisable to engage in any strenuous exercise or heavy lifting for several weeks, to allow the hernia repair to heal.